Ah…the beginning of an article. How to make it click-baity enough to get some eyeballs, yet actually offer value to the reader? Due to old-age or just lack of inspiration I’ve got nothing in this regard, so I’ll get to the story at hand:
A few weeks ago I had a sit-down with the dietetics staff at a medium sized, rural hospital. Super nice folks, very sincere. They deal with a population that is enormously overweight and which suffers from type 2 diabetes and all the related problems. This was a VERY interesting meeting as the folks who OWN the hospital are fully on-board with the Ancestral Health template and are huge advocates of things like the paleo and keto diets. The owners know this stuff works, they wanted to have a sit-down with their dietitians to try to get them on-board with the notion that eating strategies like paleo or keto “might” be helpful for their very sick (and expensive to treat) population. Everyone went around the table giving a bit of a bio and when it came to me I could see the eyes of the poor dietitians grow wide when they learned I’d written some paleo diet books and was a fan of low carb (for the right situations…you know, like fat loss and type 2 diabetes.)
Things got a bit…fidgety after my bio but our moderator did a great job of smoothing things over and asked the dietetics staff to go through what their process is in working with these obese and or type 2 diabetic patients. Again, I do not want to paint these folks as anything other than sincere and well meaning, but here is what they shared:
1-The MAIN item they focus on is getting folks to “drink more water.” This was mentioned and reiterated at least a dozen times.
2-Their avant garde initiative was to have families eat together, but a point was made that they “should not in any way criticize or second guess what they were eating” and yes, that IS a direct quote.
I want to unpack the second point first: I cannot think of a better basic recommendation that families should share meals together. Life is short, family is everything. Turning off the TV, putting away the smart-phones and other distractions and “talking” is a lost art these days.
THAT is awesome.
But…
In what was at least a 15 minute presentation, food-quality was not mentioned once. And upon inspection of the literature which supports this program, the claim was made that this mindful family eating was THE route to reversing weight and health issues that are dietary in nature.
Community IS one of the four pillars of health (along with sleep, movement and….food) but what was related to me is the vast majority of meals taken by these families were fast food, desserts, and what would generally be termed “highly processed snacks.”
Now, I do think far too much emphasis is placed on “diet.” For example, most people citing the upsides of Blue Zones focus almost exclusively on diet and pay little attention to the extended communities which are clearly a major factor in the health and well-being of these populations.
But the folks in the Blue Zones are NOT eating fast food. Ever. Not yet.
I asked these folks how they felt the program was working…as in, did they see decreasing rates of death and disease, were medical costs going down. These folks mentioned “evidence based medicine” quite frequently and I asked what one would consider to be a reasonable question about the efficacy (evidence of results) of this mindful-eating initiative. What I got was a pretty defensive back-pedaling as the unfortunate reality is the costs of dealing with all these diet and lifestyle related problems has continued its upward trend, which by the way is exponential in nature (understanding the implications of exponentials in this scenario might be worth unpacking in a future article.)
So, despite good intentions, this mindful eating program is not producing results that really matter.
You may think I’m being a big meanie here, but I’ll share an example of how this thinking is failing the population these folks are entrusted to serve. I asked for an example of one of their most challenging and expensive situations. This turned out to be a middle-aged male who is type 2 diabetic, on dialysis and he is now effectively a trunk. ONLY a trunk. Both arms have been amputated at the shoulder, both legs amputated at the hips, all due to diabetic complications. This poor guy has suffered a slew of surgeries (those limbs come off in pieces, not at once…toes, then foot, then lower leg…you get the picture) and must be medically transported multiple times per week for dialysis…then you have his medication costs and the fact he is no longer able to work and needs a full-time care provider. I won’t even relate how much this one individual has cost this system (and continues to cost) as you’d think I’m making the number up.
Fifty years ago this scenario was UNHEARD of. It did not happen. It is now commonplace…and the best “evidence based medicine” recommendations these healthcare providers can offer is “mindful eating” and an insistence that folks should not worry about their food quality. They do not want people to feel shame about what’s on their plate. Before you are Triggered and put words in my mouth, I am not advocating these people should be shamed in any way. But I do think this is an epic failure on the part of the folks tasked to educate and help these folks. Pushing for food quality is the only way this story is going to change and even doing that is going to be tough to implement when we consider the nature of our modern, hectic lives and hyper-palatable foods. Our best efforts are likely to produce lackluster results, but this is not remotely our “best efforts.”
Ok, now to point #1 from above: Drink more water.
These folks were absolutely starry eyed at this suggestion, and they did say they have seen improvements in this area. Often, “water” is interpreted as “soft-drinks” but to the point above, there is a nervousness around suggesting there may be better and worse options as it might make someone feel bad to suggest sodas, although tasty, may not be all that healthy. I asked these folks what they felt, from a medical and physiological perspective, drinking more water would do for folks.
The responses fell into two camps:
1-People are “chronically dehydrated” and this is a major health concern.
2-Drinking water “fills people up.”
To point #2 I will simply say “no, drinking more water does not cause people to spontaneously reduce caloric intake.” I’ll let you practice your Google-fu in digging up the citations on that. On point #1 I’ll refer you to this article and pull out a few highlights on heat related deaths/illness, particularly in athletic populations. Why am I using this information? People who are active tend to require more water. People in warm settings require more water. So, exercising in the heat….man, we should really see the dangerous effects of dehydration, right? Well, from the article:
The Myths of Dehydration and Heat Illnesses
- -The primary cause of hyponatremia in athletes is drinking too much water.
- -The incidence of hyponatremia appears to be between 13% and 15% among endurance athletes.
-Sodium supplementation has no effect on the occurrence of hyponatremia. - –There seems to not be a single case of death resulting from sports-related dehydration in the medical literature.
I bolded that last line and I should mention that hyponatremia is low blood salt…which is usually accomplished by consuming too much water, not too little salt.
Now, each year there are a not insignificant number of deaths/hospitalizations in the military, sporting events, hiking etc, and it is absolutely related to water…but it is generally due to TOO MUCH. I looked and looked, and what I consistently come back with is that last bolded line: One is hard pressed to find ANY examples of people dying from dehydration, even in remarkably challenging settings. People do not die and in fact do not become ill due to dehydration in the most extreme of physical activities, even in the heat…so how can one make “drink more water” the go-to recommendation for a sedentary population that spends an inordinate amount of time indoors, under near perfect temperature control?
About 700 people die each year in the US due to heat stroke. These tend to be infants, the elderly and the obese. These are populations with impaired ability to sweat and regulate body temperature. I’m not making light of that, nor am I saying that is not an important issue, but what I am saying is the focus on “drink more water” does not really address the challenges in these heat stroke examples, and appear to be not only be unhelpful, but injurious to the general athletic population.
How did this meeting wrap up? I cannot say it was a “high note.” We agreed to flesh out some common goals of educating folks about “eat whole foods” but even this seemingly benign angle on my part was met with near panic on the part of the dietetics staff.
There is a remarkable amount of energy being put into various healthcare debates, particularly in the US. These debates focus mainly on “who is going to pay” with some advocating for a system like auto insurance in which one largely pays as one goes and has a catastrophic plan for accidents, vs something folks familiar with the NHS, Canadian or Northern European models would be familiar with. I do think it’s important how we set up incentives in situations like this, but debating about who will pay for a system in which the costs of dealing with diabesity related problems are increasing exponentially and are on track to bankrupt the developed world is at best rearranging deck-chairs on the Titanic.
I will release an article on exponential costs in a week or two to provide some context here.
We face an incredibly complex problem of having a set of genetics wired for a different time, and a modern industrial food system that is a master at producing what is effectively addictive, hyper-palatable food.
If I could wave a magic wand and have every healthcare provider on the planet fully bought-in on the ancestral health model, if all these folks recognized a low carb diet can work miracles for diabesity…we’d STILL have a monumental challenge ahead of us.
We have none of that.
We have gate-keepers that are afraid to tell people “food quality matters” and the best our healthcare providers have to offer (drink more water) appears to be at best a waste of time, at worst, it may be making the problem worse.
What to do?
When I think about this two terms keep coming up: Grassroots, Trench Warfare. Grassroots means we are unlikely to see effective solutions offered up from on-high. There is too much money, inertia, ego and confusion in the dominant paradigm to just do an about-face. Grassroots means starting locally and this is where we transition to Trench Warfare: We gain ground anywhere the opportunity arises.
Although information is not generally THE thing that makes people enact significant change, if we do not have at least decent information, it’s tough to get things oriented in a way that we have any hope of success. “Drink more water” is not going to cut it. Where Grassroots meets Trench Warfare is the growing number of health practitioners who are steeped in this Ancestral Health/functional medicine model. If you’d like to learn more about this movement check out my podcast with Chris Kresser as we talk about his recently released book, Unconventional Medicine.
Via Health & Wellness http://www.rssmix.com/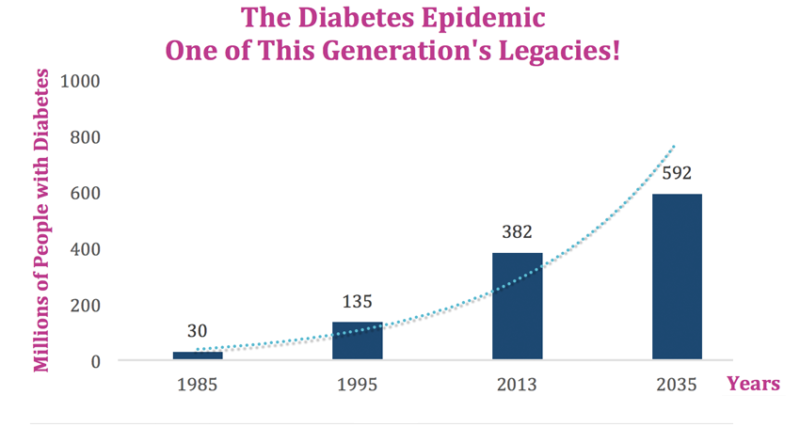
No comments:
Post a Comment